你可以有所作為。
這188bet手机app幾乎完全取決於你的捐款。
我們無法繼續與您捐贈的捐贈。
請至少將250美元的250美元捐贈給地圖集。如果沒有這一承諾,地圖集將很快要求支付認購事項,並且在世界各地的許多外科醫生都將無法進入其患者的護理依賴於它。
請立即捐款!

金宝搏188手机app最新下载,創始人188bet手机app神經外科阿特拉斯,失去了珍惜的侄女,以罕見的惡性腦腫瘤。雷切爾隻有12歲。她是G-D和純真的典型基本,其前所未有的給予和善良的自然改變了她周圍的許多人。Rachel在生活中的願景專注於改善他人的生活。跟隨她的願景,地圖集是,並將繼續致堅定的承諾,果斷地提高腦腫瘤的患者的手術護理。雷切爾永遠代表神經外科地圖集的心靈和靈魂。188bet手机app
自成立以來,地圖集積極影響全球數千名患者的照顧,這進一步加強了我們對紀念雷切爾的遺產的熱情。對於我們鼓舞人心的患者和外科醫生故事,請點擊這裏。
請加入我們支持地圖集加強雷切爾的願景!

最全麵的高級微作業技術集合。
我們廣泛的操作視頻案例集規劃了簡明的路線圖,用於執行最複雜的操作,如圖所示Aaron Cohen-Gadol。外科醫生可以在手術前的夜晚排練並發展熟練的手術策略,以獲得最佳結果。
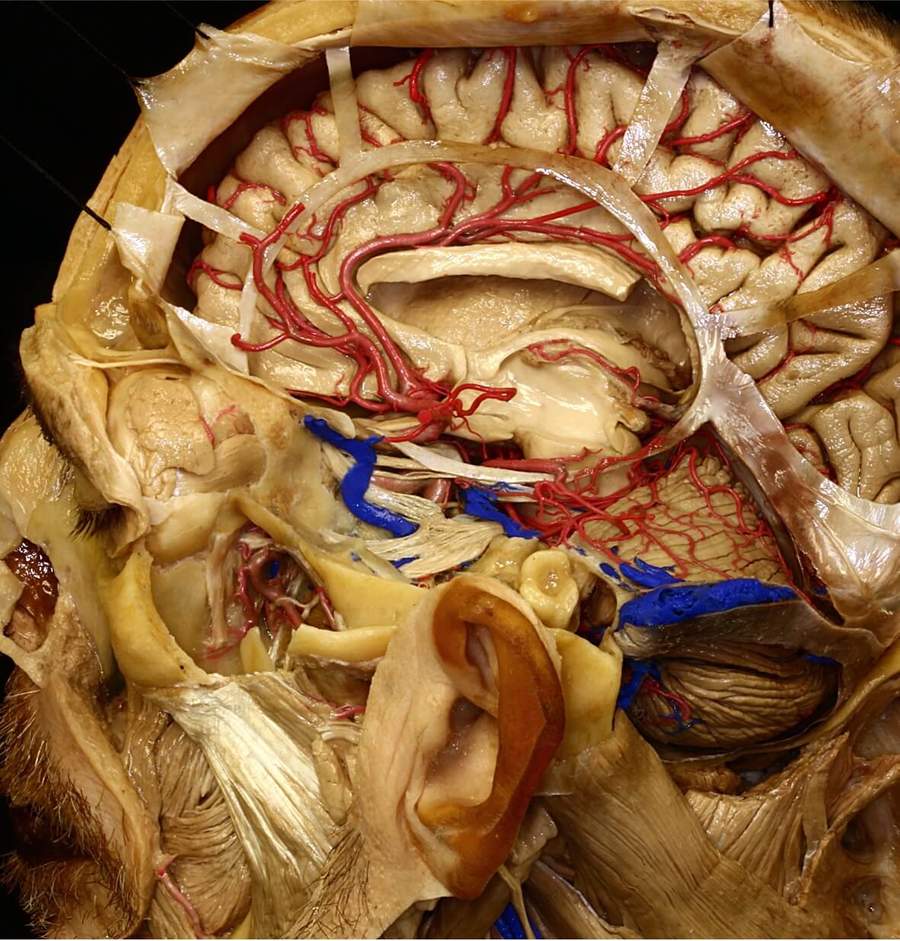
我們的神金博宝娱乐网站經腫瘤部分提供了世界上最全麵和用戶友好的神經化知識集合。大腦內的每個結構都被標記為提供對其空間取向和複雜的操作關係的深入理解。
Atlas的3D模型部分是它的唯一集合。注釋模型可以在3D中以相互作用的方式觀看或在虛擬現實(VR)空間中觀看。實現對複雜的大腦和頭骨基地操作解剖學的前所未有的理解。
這188bet手机app幾乎完全取決於你的捐款。
我們無法繼續與您捐贈的捐贈。
請至少將250美元的250美元捐贈給地圖集。如果沒有這一承諾,地圖集將很快要求支付認購事項,並且在世界各地的許多外科醫生都將無法進入其患者的護理依賴於它。
請立即捐款!
我們無法繼續與您捐贈的捐贈。請至少將250美元的250美元捐贈給地圖集。
如果沒有這種承諾,圖拉斯將很快需要付費訂閱並且在世界各地的許多外科醫生將無法進入,其患者的護理依賴於它。請立即捐款!